The wearable healthcare revolution is ready to deliver healthier outcomes
Wearable healthcare devices have the potential to enable better use of health data in research and innovation as well as intervention and services, believes Andrew Baker, managing director, Industrial and Healthcare business unit, Maxim Integrated
The traditional, centralised model of healthcare has not changed much since formal healthcare was first introduced. When someone gets sick, they go to the doctor for treatment, return home to recover, and repeat the cycle if symptoms return. In light of skyrocketing healthcare costs, combined with factors such as growing population numbers and extended life expectancies, this model does not seem sustainable.
Spending on global healthcare is expected to top US$10tn by 2022, according to the 2019 Global Health Care Outlook report by analysts at Deloitte. As a result, healthcare providers, insurance companies, and governments are seeking ways to reduce healthcare costs while also improving the quality of care. Emerging healthcare technology is providing an answer by taking the approach of shifting care closer to the consumer and away from the old centralised service model. Wearable healthcare technologies, in particular, are poised to transform this model into one that is more personalised, proactive, and preventive.
Wearable healthcare
Worldwide shipments of wearable healthcare devices are projected to reach nearly 98 million units annually by 2021, according to the market intelligence firm, Tractica. From patches to bands, watches, and even jewellery, devices that continuously monitor vital signs can support patients with alerts that help them better manage chronic diseases or identify previously undetected conditions. For people with limited access to healthcare, such as those living in rural areas, a wearable device coupled with a tele-medicine system can help physicians provide remote monitoring and care. By potentially improving outcomes, these technologies can enable healthier lives and reduce healthcare costs. The Deloitte report notes, “Digital technologies are supporting health systems’ efforts to transition to new models of patient-centered care and ‘smart health’ approaches to drive innovation, increase access and affordability, improve quality, and lower costs. Digital solutions also have the potential to enable better use of health data in research and innovation to support personalised health care, better health interventions, and health and wellness services.”
 Figure 1: Smartwatches are an example of wearable healthcare devices. They continuously monitor specified parameters and provide real-time data. (Photo courtesy of Andrey Popov/Shutterstock)
Figure 1: Smartwatches are an example of wearable healthcare devices. They continuously monitor specified parameters and provide real-time data. (Photo courtesy of Andrey Popov/Shutterstock)
Smartwatches are just one of many types of wearable healthcare devices that are providing actionable insights from continuous, real-time monitoring of various health parameters (Figure 1).
Wearables making waves
Heart monitoring patches are already available for doctors to prescribe. An example of a use case where a wearable can make a profound impact is atrial fibrillation, or AFib. An AFib is an irregular heartbeat that can lead to blood clots, stroke, heart failure and other heart-related complications. One recent study of the condition estimates that 33.5 million people, worldwide, had AFib in 20104. Many people with the condition are asymptomatic, however, so screening is critical to ensure that these individuals are provided with the necessary recommendations and care.
The way that screening is performed is significant. A screening conducted during an annual physical may not catch any irregularities because the tell-tale signs can occur sporadically. Continuous monitoring provides a better approach. In a study of more than 5,200 people in the US with risk factors for AFib, one third wore a monitoring patch to collect electrocardiogram (ECG) data for up to two weeks. The other two thirds were the comparison group that received conventional care, typically with routine visits to their doctor. At the end of the year-long study, 109 people wearing the patches were diagnosed with AFib compared to 81 people in the group that was not being continuously monitored.
Diabetes management is another area that is on the cusp of being transformed via continuous glucose monitoring (CGM). There is a variety of solutions that presently exist and there are others in development. Existing CGM is in the form of a patch worn on the body that uses a micro-needle to penetrate below the skin to measure the concentration of glucose in the interstitial fluid. The measurements are either stored on the device to be read out using an NFC radio or are transmitted in real-time to a smartphone or smartwatch via Bluetooth. CGM can transform the lives of Type 1 diabetics, giving them more control over their condition and enabling closer monitoring and control of their glucose levels. CGM is now being offered to Type 2 diabetics to improve their management of the condition and provide relief from finger-stick tests throughout the day. In fact, these devices may be sold over the counter in the not too distant future. This level of availability will open up new use cases such as dietary monitoring. Many researchers and development teams are working on new technologies to enable non-invasive solutions to replace the existing minimally invasive patch solutions used today. One example of this is happening at the University of Bath in the UK, where researchers are developing a patch that measures and monitors blood sugar levels with an array of miniature sensors to take blood sugar readings every 10 to 15 minutes over several hours, drawing glucose out from fluid between cells across hair follicles. The researchers have a proof of concept but their technology still must undergo clinical trials and more before it is ready for the real world6.
Epilepsy management
Epilepsy is another condition where continuous monitoring can flag the most dangerous types of seizures, providing alerts to caregivers. In early 2018, the US Food and Drug Administration approved the Embrace smartwatch from Empatica for neurological use. The Cambridge, Massachusetts-based company uses sensors and machine learning technology to measure electrodermal activity and identify when the wearer is experiencing a ‘grand mal’ seizure. This triggers text or email alerts to designated care givers. In a multi-site clinical study, the Embrace watch detected 100% of the seizures experienced by participating patients.
These are just a few examples of the wearable health innovations that are on the market now or due to be soon; putting more actionable data into the hands of patients and healthcare providers.
 Figure 2: Electronic health records are part of the wave of digitisation that is transforming healthcare. (Photo courtesy of metamorworks/Shutterstock)
Figure 2: Electronic health records are part of the wave of digitisation that is transforming healthcare. (Photo courtesy of metamorworks/Shutterstock)
Countries around the world are taking action to foster digital health technology innovation. The US is the largest market for wearable healthcare devices, and the Food and Drug Administration (FDA) is encouraging digital health innovation via its Digital Health Innovation Action Plan. As part of this plan, the announced in 2017, a digital health software pre-certification pilot program that evaluates software developers or digital health technology developers, rather than placing the main focus on the product itself. The FDA reviews systems for software design, validation, and maintenance and pre-certifies companies once it has determined that they have met established quality standards.
While the European market has been slower than the US to adopt wearable health devices, there are indications—including movements toward digital health models—that it could catch up soon. In the EU (European Union), there is a project called SENDoc, which is evaluating the use of wearable sensors in ageing populations based in remote areas. Specifically, the sensors are measuring mobility, strength, and balance as part of an effort to support independent living in rural areas.
In the Asia-Pacific region, the wearable medical device market is projected to maintain a CAGR of 15.94% until 2023, according to Market Research Future. The researchers do note, however that device cost may be a restraint on market growth there.
Low power ICs drive adoption
What will it take to make checking health vitals as easy as checking the daily weather? An ideal medical wearable is comfortable and unobtrusive; runs for a long time between charges; provides a simple user interface (or automatically uploads collected data to the cloud for access via a smartphone app) and delivers accurate information without requiring the wearer to do anything differently.
Based on these criteria, the underlying technology inside these devices needs to be tiny, with low power consumption and low heat dissipation. A high level of integration would address the size constraints, and, of course, the bio-sensors must be highly accurate.
Semiconductor vendors are playing an important role in bringing wearable health devices to life by designing ICs that meet these criteria. Tiny, low-power microcontrollers provide processing power, efficient and compact power management ICs regulate voltage levels, and fuel-gauge ICs contribute to battery health. Analogue front-ends (AFEs) deliver electrocardiogram (ECG) waveforms, while ultrasound imaging transceivers and receivers play important roles in imaging systems. Sensors can monitor photoplethysmography (PPG), body temperature, and other vitals. There are now even biosensor modules for wearables that integrate multiple parameters, such as synchronised PPG and ECG monitoring.
For faster prototyping of wearable health designs, designers can turn to development platforms integrated with various components. Maxim, for example, recently introduced its Health Sensor Platform 2.0, believed to be the first wrist-worn, low power platform for monitoring ECG, heart rate, and temperature. The platform consists of a PPG AFE sensor, a bio-potential AFE, a human body temperature sensor, a microcontroller for wearables and IoT applications, a wearable power-management IC and a biometric sensor hub with embedded heart-rate algorithm (Figure 3). The open platform allows designers to use it to evaluate their own algorithms; it can save up to six months in development time.
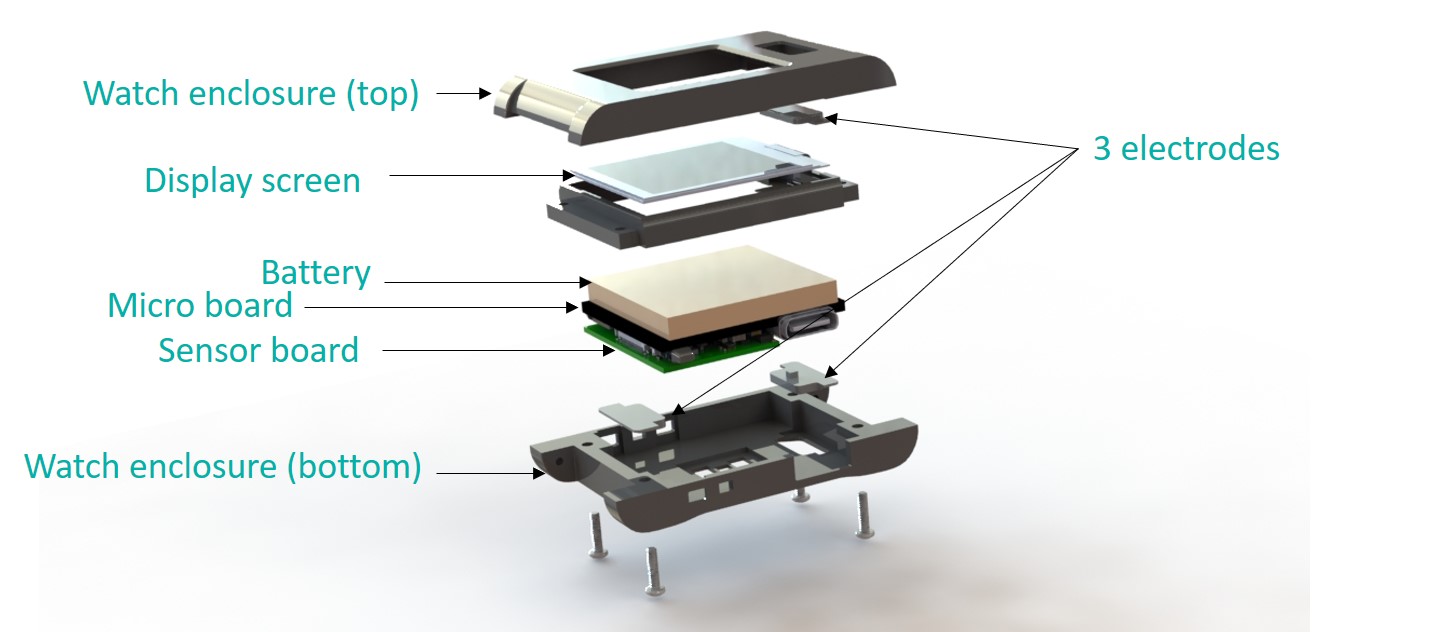 Figure 3: Maxim believes its Health Sensor Platform 2.0 is the first low power platform for monitoring ECG, heart rate, and temperature, designed to be worn on the wrist
Figure 3: Maxim believes its Health Sensor Platform 2.0 is the first low power platform for monitoring ECG, heart rate, and temperature, designed to be worn on the wrist
The future prognosis
For wearables to truly revolutionise healthcare, changes in hospital infrastructures and workflows will need to take place to support mass adoption. Data collected by wearables can be uploaded to the cloud and shared with healthcare providers, allowing them to remotely monitor their patients. These providers will need to have the means to promptly evaluate the data and also to keep it secure. As artificial intelligence (AI) algorithms become more sophisticated, there may come a time when these algorithms are able to accurately identify potential areas for healthcare providers to review more closely, so that they will not have to review all of the data; perhaps there may even be a time when AI can be used to diagnose conditions.
At the moment, wearable healthcare devices are giving us valuable insights to help us manage our well-being. Down the road, these technologies could play a larger role in facilitating healthier outcomes for more people while also lowering healthcare costs.